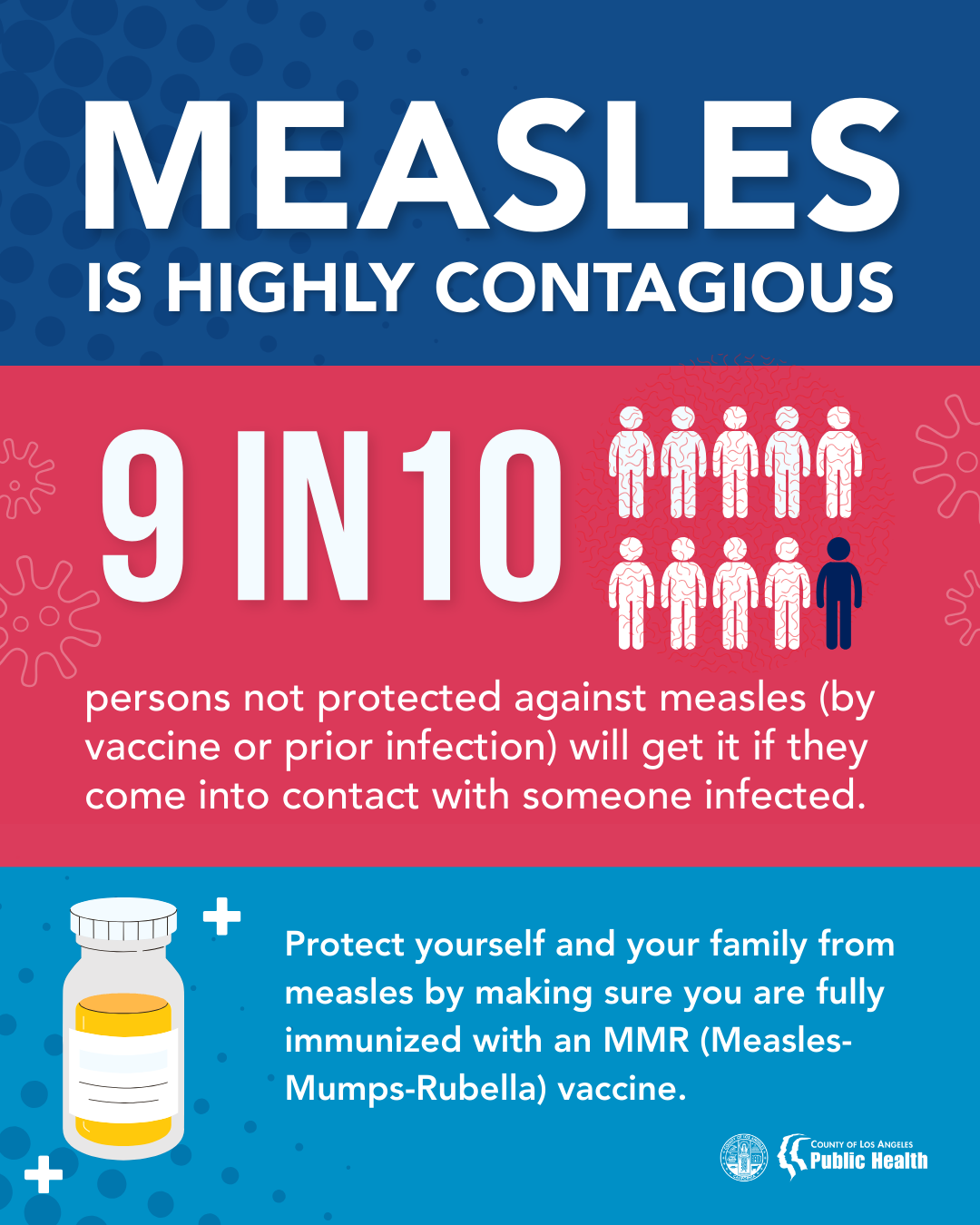
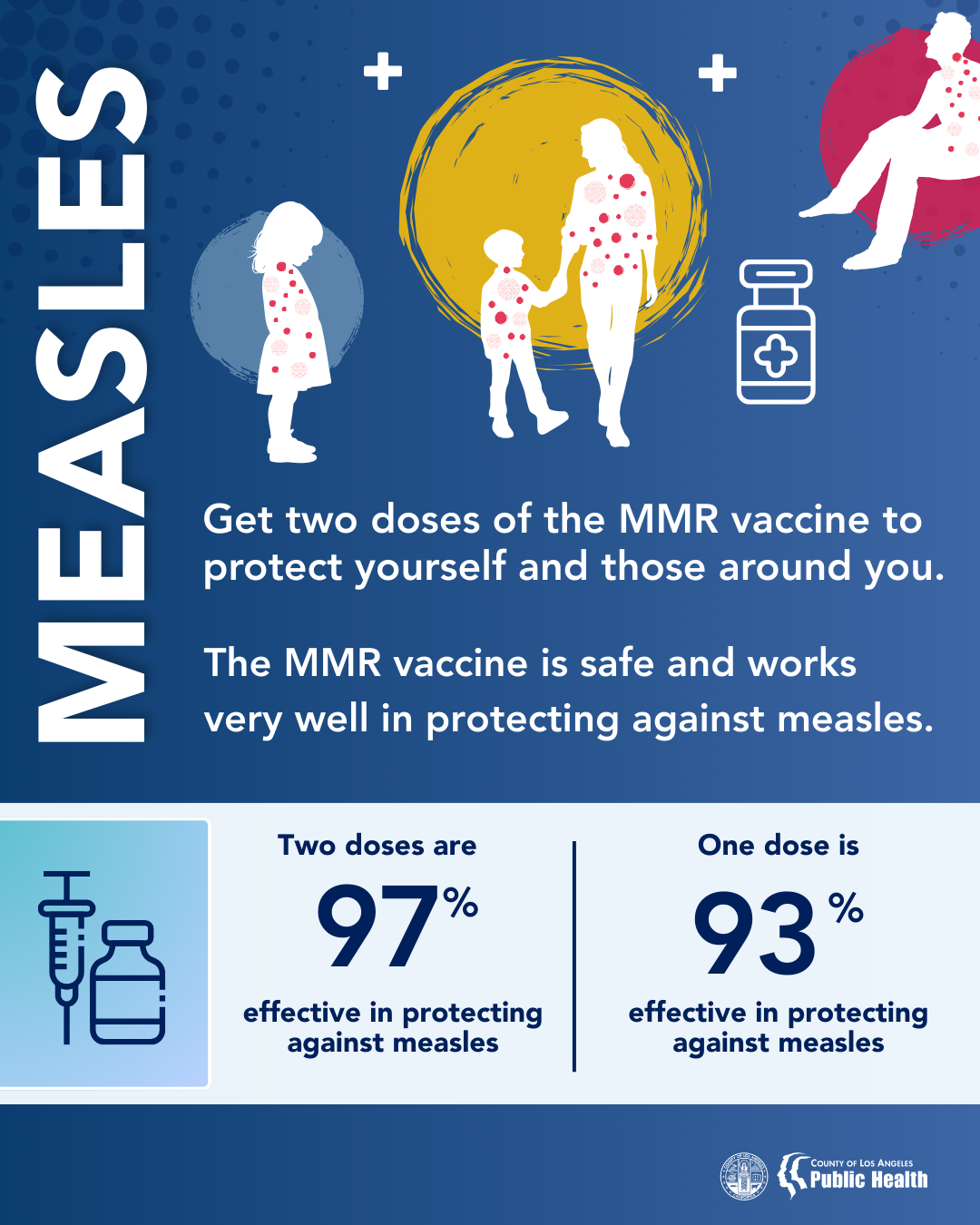
If you are an adult who is planning international travel or traveling within the United States in known measles outbreak areas, you should get vaccinated against measles if you did not receive 2 doses as a child.
If your child is 6-11 months old and you’re planning international travel or traveling to an area in the United States experiencing an outbreak, you should speak to your child’s provider to get an early dose of vaccine against measles. After that, your child should follow the recommended schedule and get:
- Another dose at 12 through 15 months.
- A final dose at 4 through 6 years.
If you are or your child is 12 months old or older and planning international travel or traveling to an area in the United States experiencing an outbreak, you should receive your first dose of vaccine against measles immediately. You can get a second dose as soon as 4 weeks after your first dose.
You should plan to be fully vaccinated against measles at least 2 weeks before you depart. If your trip is less than 2 weeks away and you're not protected, you should still get a dose of MMR.
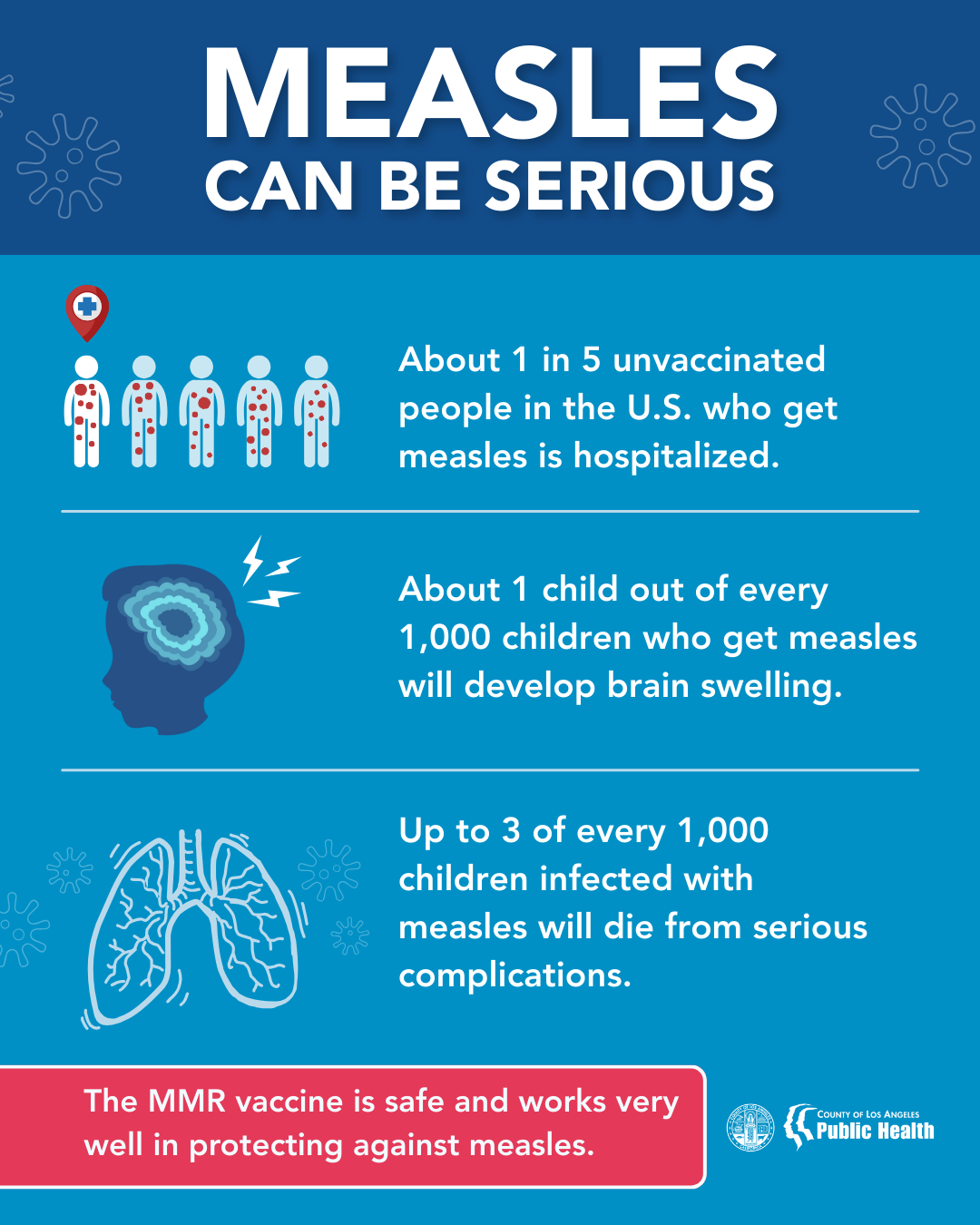
Watch your health for 3 weeks after you return from your trip. Measles is very contagious and can spread to others through coughing and sneezing.
Call your doctor immediately if you or your child gets sick with a rash and fever. Tell your doctor you traveled abroad, and whether you have received MMR vaccine.
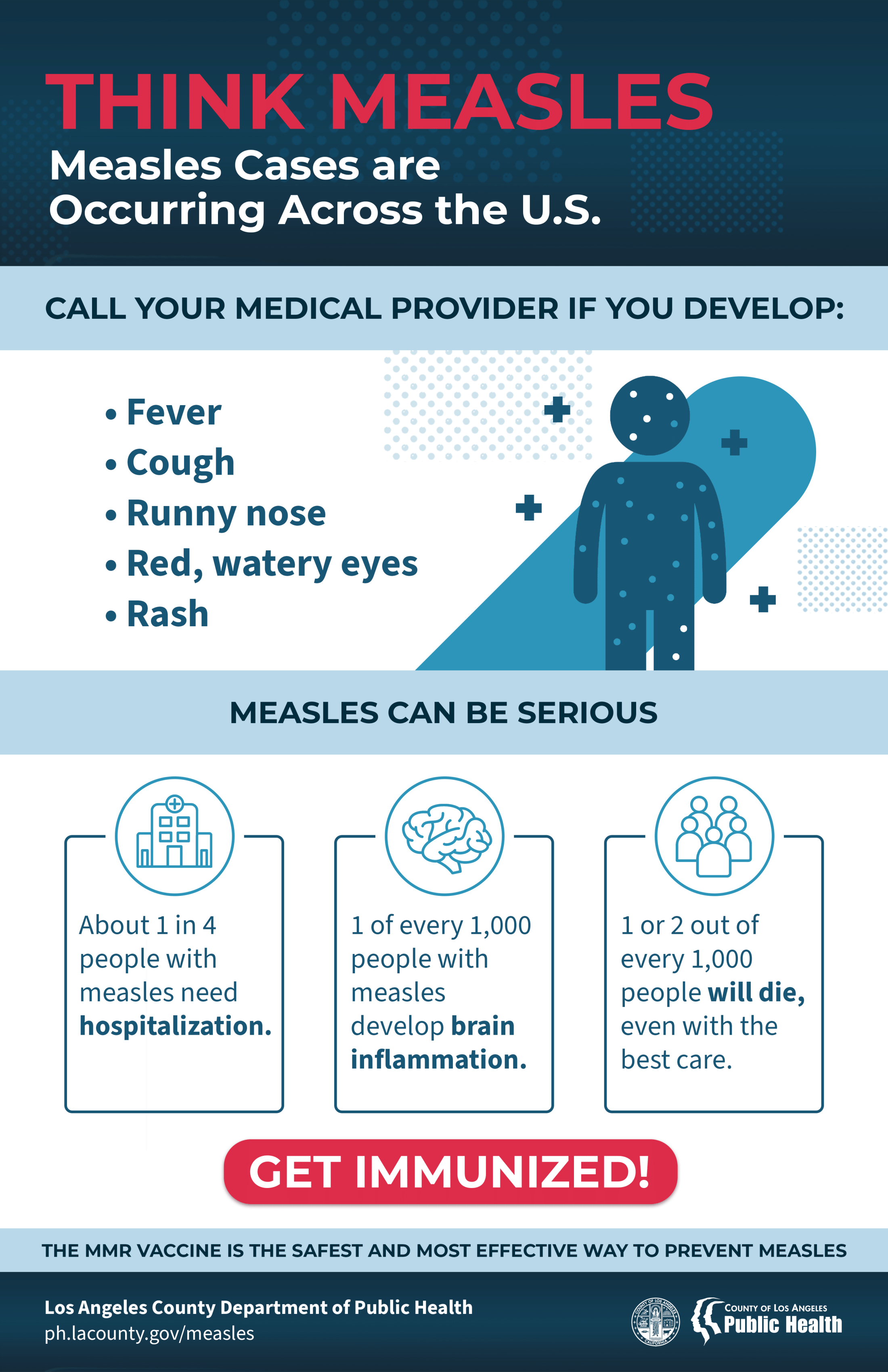
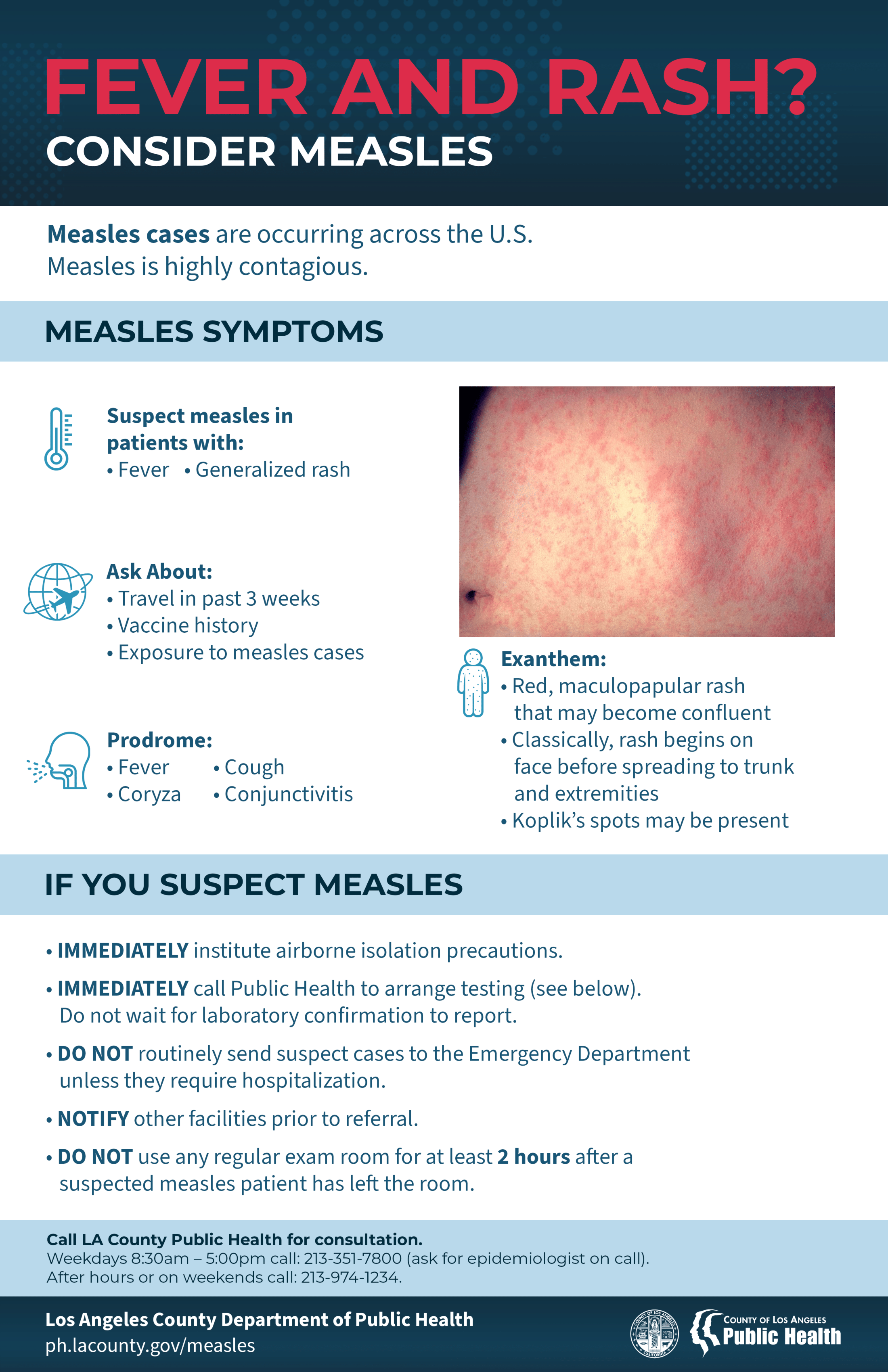
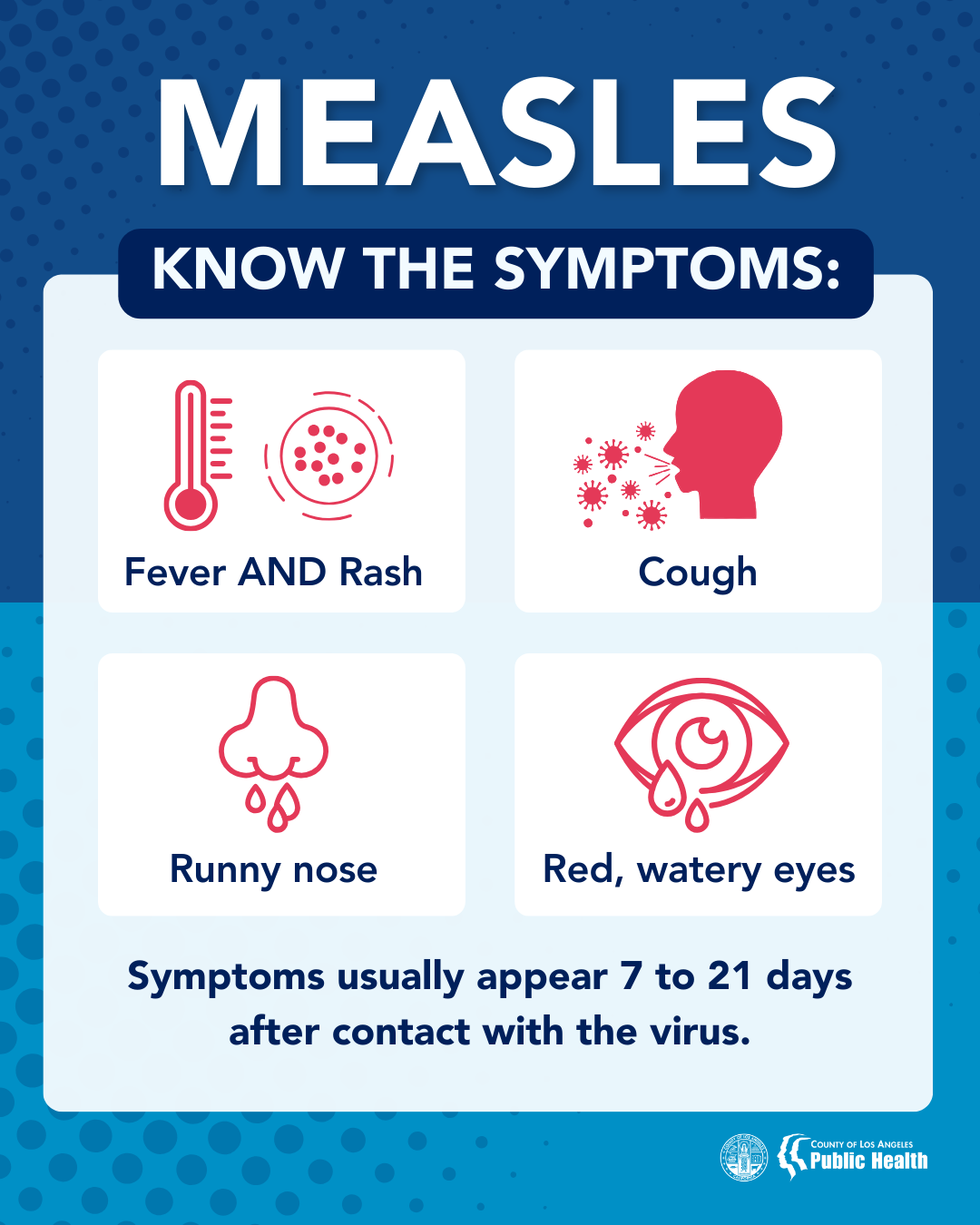
- Measles symptoms typically include:
- High fever (may spike to more than 104° F)
- Cough
- Runny nose (coryza)
- Red, watery eyes (conjunctivitis or pink eye)
- Rash (starts 3-5 days after other symptoms start)