Prevention & Guidance
Mpox
Residents can call the Public Health Call Center for more information on Mpox, including general information, testing, treatment, and vaccines:
Open 7 days a week 8:00 a.m. – 8:00 p.m.
The main way Mpox has been spreading is through close, intimate contact with symptomatic people, mainly during sexual activity.
Mpox can be spread by:
- Direct skin-to-skin contact with the sores or scabs from a person with Mpox.
- Direct contact with the body fluids or respiratory secretions from a person with Mpox, such as drainage from skin sores or saliva that was in contact with mouth sores.
- Getting stuck/punctured by a sharp object (such as a needle) that has touched the sores or body fluids of a person with Mpox.
- Touching materials (such as bedding, towels, clothing) that touched the sores or body fluids of a person with Mpox and have not been cleaned. (Note: the CDC states that the risk of getting Mpox this way is low).
A person with Mpox can spread it to others from 4 days prior to the day symptoms start until the rash has fully healed and a fresh layer of skin has formed. This usually takes 2 to 4 weeks.
A pregnant person with Mpox can spread the virus to their fetus through the placenta. The virus can also be spread to the baby by close contact during and after birth.
Scientists are still researching more about how Mpox is spread, including:
- If the virus can be spread when someone does not have symptoms (so far there is no evidence that this is happening)
See CDC How Mpox Spreads for additional information.
Anyone, regardless of sexual orientation or gender identity may contract Mpox through close personal contact with someone who has symptoms of Mpox. Data suggests transmission has occurred primarily through close-knit social networks of gay, bisexual, and other men who have sex with men through intimate contact. Men who have sex with men, particularly those with multiple or anonymous sexual partners, face a heightened risk of exposure.
There are several ways to reduce the risk of Mpox:
- Get vaccinated with two doses of the Jynneos vaccine.
-
Avoid very close, intimate contact with someone with Mpox symptoms, especially:
- Oral, anal, and vaginal sex, or touching the genitals or anus
- Hugging, cuddling, massaging, and/or kissing
- Skin-to-skin contact with the rash on their body
- Sharing towels, clothing, bedding, blankets, or other objects and materials (e.g., toothbrushes, cups, utensils, and sex toys) that have not been cleaned.
- Wash your hands, fetish gear, sex toys, and any fabrics (bedding, towels, clothes) after having sex.
- Wear appropriate protective equipment (mask, gloves, and gown) if you cannot avoid close contact with someone who has Mpox symptoms.
- Talk to sexual partner(s) about any recent illness and new or unexplained sores or rashes including on the genitals or anus.
- Use a condom. Condoms alone are likely not enough to prevent Mpox. But they might reduce the risk, and may help prevent sores in sensitive areas, like the anus, mouth, or genitals.
- Reduce the number of sex partners.
- Avoid riskier activities such as anonymous sex and sex parties.
For more information see the CDC webpage, Safer Sex, Social Gatherings and Mpox.
Mpox is a contagious disease caused by the Mpox virus. The Mpox virus is in the same family of viruses as variola, the virus that causes smallpox. Mpox and smallpox symptoms are similar, but Mpox symptoms are milder and rarely fatal. Mpox is not related to chickenpox.
Mpox (originally called “monkeypox”) was first discovered in 1958 in colonies of monkeys kept for research. The first case in humans was recorded in 1970. Previously, Mpox had been reported in people in several central and western African countries. Almost all Mpox cases in people in the United States were linked to international travel to countries where the disease is known to occur or through imported animals.
Since May 2022, however, there has been a large outbreak of Mpox in many countries, including the United States. The main way people are becoming infected is through close, intimate contact with symptomatic people, mainly during sexual activity. While some people can get very sick, most people do not need hospital care and recover in 2-4 weeks. Vaccines and antiviral treatment are available for Mpox.
The following Frequently Asked Questions (FAQs) are about the US 2022 Mpox outbreak.
Updated 12/1/22
Symptoms usually start 5-21 days after exposure.
Most people recover in 2-4 weeks.



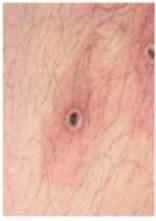


All of the above images are from GOV.UK, https://www.gov.uk/guidance/mpox
Mpox symptoms usually start within 3 weeks of exposure to the virus.
The most common symptom is a rash that may:
- Look like bumps, pimples, blisters, or scabs and will go through several stages before healing. Generally, the rash starts as red, flat spots, and then becomes bumps. Those bumps can then become filled with fluid which turns to pus. The bumps then crust into a scab.
- Be on or near the genitals (penis, testicles, labia, and vagina), anus (butthole), mouth, or other areas like the hands, feet, chest, and face.
- Spread over the body or it may be limited to one area. There may be just a few bumps or blisters.
- Be painful and/or itchy. Some people have severe pain, especially if the rash is inside their mouth or anus.
In addition to the rash, people may also develop flu-like symptoms. These can appear 1-4 days before the rash starts or after the rash starts. They include fever/chills, swollen lymph nodes, exhaustion, muscle aches, and headache.
Most people with Mpox recover in 2-4 weeks.
The main way Mpox has been spreading is through close, intimate contact with symptomatic people, mainly during sexual activity.
Mpox can be spread by:
- Direct skin-to-skin contact with the sores or scabs from a person with Mpox.
- Direct contact with the body fluids or respiratory secretions from a person with Mpox, such as drainage from skin sores or saliva that was in contact with mouth sores.
- Getting stuck/punctured by a sharp object (such as a needle) that has touched the sores or body fluids of a person with Mpox.
- Touching materials (such as bedding, towels, clothing) that touched the sores or body fluids of a person with Mpox and have not been cleaned. (Note: the CDC states that the risk of getting Mpox this way is low).
A person with Mpox can spread it to others from 4 days prior to the day symptoms start until the rash has fully healed and a fresh layer of skin has formed. This usually takes 2 to 4 weeks.
A pregnant person with Mpox can spread the virus to their fetus through the placenta. The virus can also be spread to the baby by close contact during and after birth.
Scientists are still researching more about how Mpox is spread, including:
- If the virus can be spread when someone does not have symptoms (so far there is no evidence that this is happening)
- How often it spreads through respiratory secretions
- Whether Mpox can be spread through semen, vaginal fluids, urine, or feces.
See CDC How Mpox Spreads for additional information.
Updated 11/2/22In this current outbreak in the U.S., the vast majority of people diagnosed with Mpox are men who reported having sexual or close intimate contact with other men. But anyone, regardless of their sexual orientation or gender identity, is at risk if they have close, intimate skin-to-skin contact with someone with symptomatic Mpox.
As this is a new outbreak, public health organizations nationally and internationally are still learning about the situations or behaviors that may put people at increased risk. We will continue to share information as we learn more. More information is in the CDC Science Brief: Detection and Transmission of Mpox Virus.
Updated 11/2/22There are no FDA approved medicines to specifically treat Mpox. But an FDA approved antiviral medicine used to treat smallpox called tecovirimat (or TPOXX) can be used to treat people with Mpox. TPOXX can be given to people with severe Mpox, including lesions in sensitive areas or pain that is not controlled with over-the-counter remedies. It can also be given to people who are more likely to get severely ill (see Who is at higher risk for getting very sick? below). Learn more at CDC Learn more at CDC Tecovirimat (TPOXX) for Treatment of Monkeypox.
If you have Mpox, your doctor can also prescribe non-Mpox medicines that can help reduce pain and irritation from the rash or sores. For information on how to manage your symptoms, visit the CDC webpage What to Do If You Are Sick.
Updated 11/2/22Many people with Mpox have a mild illness, but for some people Mpox can be serious. Signs of severe Mpox can include:
- Rash or sores on or near the eyes
- Rash that spreads all over the body or blend together
- Pain in the rectum (butt) or urethra (pee hole) that makes it hard to go to the bathroom
- Pain in the mouth that makes it hard to eat and drink
- Rash that is bleeding or looks infected
- Symptoms that get worse or do not improve over time
Seek medical help right away if you get any of these symptoms or have other symptoms that concern you. If you have uncontrolled or advanced HIV, see a doctor right away, even if your Mpox symptoms seem mild.
Updated 11/2/22People living with uncontrolled or advanced HIV are at high risk for becoming severely ill if they get Mpox. Other people who are very immunosuppressed are also considered high risk for becoming very ill.
People with Mpox who have lesions in their eyes, mouth, rectum, and/or genitals can have severe pain and swelling. These areas can become infected with bacteria. There is also a risk of scarring.
In addition, based on what we know from previous Mpox outbreaks, the following groups may be at higher risk for getting severe Mpox, if they become infected. We don’t yet know the extent of their risk for getting very sick if infected during the current outbreak.
- People who are immunosuppressed (have a weak immune system because of a treatment, disease, or infection).
- People with a disease or condition that affects the skin such as eczema, atopic dermatitis, psoriasis, impetigo, severe acne, herpes, or burns.
- Children, particularly those who are under 8 years of age.
- People who are pregnant or breastfeeding.
During this outbreak, most of the people with Mpox have been adult men who have not required hospitalization. However, there have been very severe Mpox cases, including some deaths, in people with severely immunocompromised immune systems. This includes people living with untreated or uncontrolled HIV infection.
Updated 11/2/22Contact your doctor right away if you have a new, unexplained, rash or lesions on any part of your body. This is especially important if you were exposed to someone with Mpox or suspected to have Mpox. Cover all parts of the rash with clothing, gloves, and/or bandages and take steps to protect others. These include avoiding skin to skin contact and being physically intimate with others until you have been checked out by a doctor. Be sure to wear a mask when you see a doctor.
Call the Public Health Call Center at 1-833-540-0473 (open daily 8:00 am to 8:30 pm) if you don’t have a doctor or health insurance. If you have a rash, you can also access services at Public Health’s Sexual Health Clinics (see schedule here).
Until you know you don’t have Mpox, take steps to reduce the risk of spreading the infection by staying away from others. See Isolation Instructions for People with Mpox.
Updated 11/2/22If you have a rash that might be due to Mpox, your doctor will evaluate you. Based on their assessment, they may swab your rash for testing. The swabs are sent to a lab, and the test result should be available in a few days. There are no self-tests or home tests for Mpox at this time.
Until you know you don’t have Mpox, it is important to follow Mpox isolation instructions.
Updated 11/2/22If you have been diagnosed with Mpox, you should isolate to protect others. Follow the Isolation Instructions for People with Mpox which are available in several languages at ph.lacounty.gov/mpox.
Contact your sex partners and any people you had very close, intimate and/or prolonged contact with since your symptoms started. Do this as soon as possible so they can consider getting vaccinated (if they have not already had Mpox or not already been vaccinated for Mpox). Getting vaccinated after exposure may prevent Mpox or make the illness less severe. They can also look out for any symptoms of Mpox.
Please answer calls from Public Health. They will be in touch to ask you about your activities before and after you developed symptoms. This is to try to find out how you may have been exposed to Mpox and to help to identify other people who may have been exposed.
Updated 11/2/22There are a number of ways to reduce the risk of Mpox:
- Get vaccinated if you are eligible (see below)
- Avoid very close, intimate contact with someone with Mpox symptoms, especially:
- Oral, anal, and vaginal sex, or touching the genitals or anus
- Hugging, cuddling, massaging, and/or kissing
- Skin-to-skin contact with the rash on their body
- Sharing towels, clothing, bedding, blankets, or other objects and materials (e.g., toothbrushes, cups, utensils, and sex toys) that have not been cleaned.
- Wash your hands, fetish gear, sex toys, and any fabrics (bedding, towels, clothes) after having sex.
- Wear appropriate protective equipment (mask, gloves, and gown) if you cannot avoid close contact with someone who has Mpox symptoms.
- Talk to sexual partner(s) about any recent illness and new or unexplained sores or rashes including on the genitals or anus.
- Use a condom. Condoms alone are likely not enough to prevent Mpox. But they might reduce the risk, and may help prevent sores in sensitive areas, like the anus, mouth, or genitals.
- Reduce the number of sex partners.
- Avoid riskier activities such as anonymous sex and sex parties.
For more information see the CDC webpage, Safer Sex, Social Gatherings and Mpox.
Updated 11/2/22Yes. A vaccine called JYNNEOS is FDA approved to prevent Mpox in people ages 18 and over. It is also available under FDA emergency use authorization (EUA) for people under age 18. It is a two-dose vaccine. It takes 14 days after getting the second dose of JYNNEOS to get the best immune response to the vaccine. But even getting one dose can provide some protection. It is important to note, neither one nor two doses of vaccine are 100% effective at preventing infection. It is still important to continue to take other steps to reduce your risk.
If the vaccine is given before a person is exposed to Mpox, it helps to protect them from getting Mpox.
If it is given after exposure, it may help to prevent the disease or make it less severe. It should be given within 14 days of exposure (ideally in the first 4 days).
If someone already has Mpox the vaccine is not recommended. For more information about the vaccine, see Mpox vaccine FAQs.
Updated 11/2/22The JYNNEOS vaccine is FDA approved to prevent mpox disease in people aged 18 years and older. It is also available under FDA emergency use authorization (EUA) for people under aged 18 years. For more detailed information about eligibility, please visit ph.lacounty.gov/mpoxvaccine.
Updated 7/8/25
- If you have insurance, talk to your doctor or check with your local pharmacy to see what vaccines are offered. If you are an uninsured or underinsured adult, you may be able to access JYNNEOS vaccine at no cost at select locations that carry the vaccine, including federally qualified health centers and public health sites. You may also search MyTurn to locate a vaccine provider near you.
- To find a vaccination site near you, visit ph.lacounty.gov/vaccines
Track your health. People who develop Mpox usually get symptoms 7-14 days (and up to 21 days) after being exposed. You can continue your routine daily activities as long as you do not develop symptoms. Be prepared to isolate yourself from others if you develop Mpox symptoms.
Get vaccinated if you have not already completed a two-dose Mpox series. Getting a dose of Mpox vaccine within 4 days after exposure can help prevent you from becoming infected. Getting a vaccine 4-14 days after exposure may make your infection less severe. Learn more at http://ph.lacounty.gov/ip/diseases/mpox/index.htm.
Please answer calls from Public Health. If you are named as a contact to someone with mpox, Public Health may be in touch with you to see how you are feeling and to offer vaccination if appropriate.
Follow Guidance for Individuals Who Have Been Exposed to Mpox for more information.
Updated 7/8/25People living with HIV should follow the same recommendations as everyone else to protect themselves from getting Mpox. However, there are additional steps that people with HIV should take. This is because there is more and more evidence that Mpox infection can be more severe for people living with HIV who have low CD4 counts (<350 cells/ml) or an unsuppressed viral load.
What can you do to protect yourself?
- Get the Mpox vaccine. The vaccine is safe and can be given either between the layers of the skin (intradermally) or beneath the skin (subcutaneously).
- Avoid direct contact with the rash or secretions of people with Mpox. See How can I reduce my risk of getting Mpox?
- Make sure that you have your HIV infection under control. It is important that you take your antiretroviral therapy (ART) regularly as instructed. If you need assistance with finding an HIV doctor or making an appointment, Public Health staff are available to help - visit ph.lacounty.gov/dhsp/RapidART.htm or call 1-833-351-2298.
What should you do if you think you may have Mpox?
- If you do develop a new rash or sores that you think may be Mpox, see a doctor right away. Let them know you have HIV.
- If your doctor suspects Mpox, they may start you on antiviral treatment for Mpox (TPOXX) right away, especially if you have uncontrolled or advanced HIV. If your HIV is well controlled but you have Mpox lesions in your eyes, mouth, rectum, or penis, they may recommend starting TPOXX to lower the risk of pain, infection, and scarring.
- If you are prescribed TPOXX, it is very important that you take it as instructed.
- For more information see What should I do if I think I have Mpox?
Visit HIV.gov Mpox Update for more information about Mpox and HIV.
Updated 11/2/22Yes. Anyone can get Mpox if they have close, personal or intimate contact with someone who has Mpox. The risk of children getting infected with Mpox during this outbreak is very low. While cases in children have happened in the U.S., they are very rare.
Younger children are at risk of getting Mpox if they live with someone who has Mpox, especially if there is any skin-to-skin contact with the infected person. If you have Mpox or suspected Mpox, take steps to protect everyone in your home. See Isolation Instructions for People with Mpox.
Adolescents who are physically intimate/sexually active with others may also at higher risk of getting Mpox. This is especially true if they are males having sex with other males. For more information see the CDC webpage, Safer Sex, Social Gatherings and Mpox.
Updated 11/2/22The U.S. Environmental Protection Agency (EPA) has a list of disinfectant products that are registered for use against the Mpox virus. The list includes popular products that many businesses and individuals already use. It can be found on the EPA website. The website has a search tool where you can look up disinfectants by different factors such as product name, contact time, and surface type.
- Check that the product is EPA-registered.
- Read the manufacturer’s directions. Make sure this is the right product for your surface.
- Clean the surface with soap and water if the directions mention pre-cleaning before applying disinfectant or if the surface is visibly dirty. Dirt can keep the disinfectant from working.
- Follow the contact time instructions. The surface should remain wet for the amount of time stated in the instructions to be effective. Reapply if needed.
Regular laundry detergents can be used for cleaning clothes or linens (e.g., bedding and towels) used by someone with Mpox.
Soiled dishes and eating utensils can be washed in a dishwasher with detergent and hot water or by hand with hot water and dish soap.
See CDC Cleaning and Disinfecting Your Home, Workplace, and Other Community Settings for more information and tips about cleaning during and after Mpox.
Updated 11/2/22Los Angeles County, Department of Public Health
ph.lacounty.gov/mpox
http://ph.lacounty.gov/ip/diseases/mpox/index.htm
Centers for Disease Control and Prevention
cdc.gov/poxvirus/mpox/index.html
California Department of Public Health
cdph.ca.gov/Programs/CID/DCDC/Pages/Mpox.aspx